Facts….
Breast cancer burden…
The American Cancer Society’s estimates for breast cancer in the United States for 2018 are:
-About 266,120 new cases of invasive breast cancer will be diagnosed in women.
-About 63,960 new cases of carcinoma in situ (CIS) will be diagnosed (CIS is non-invasive and is the earliest form of breast cancer).
-About 40,920 women will die from breast cancer
-1 in 8 women will be diagnosed with breast cancer in their life time
Why screen for breast cancer?
The prime reason for Breast cancer mortality is diagnosis at an advanced stage of disease. The rationale of a breast cancer screening program then is primarily to detect cancer when it is small and impalpable. Treatment of such screen detected small non-palpable breast cancers provides an opportunity for curing cancers by local therapy alone. Figure 1.
Is Mammography effective?
-For women 40–74 years of age who actually participate in mammographic screening every 1–2 years, breast cancer mortality is reduced by 40%.
-In one study among 609 confirmed breast cancer deaths, 71% were among unscreened women (Cancer 2014; 120:2839–2846).
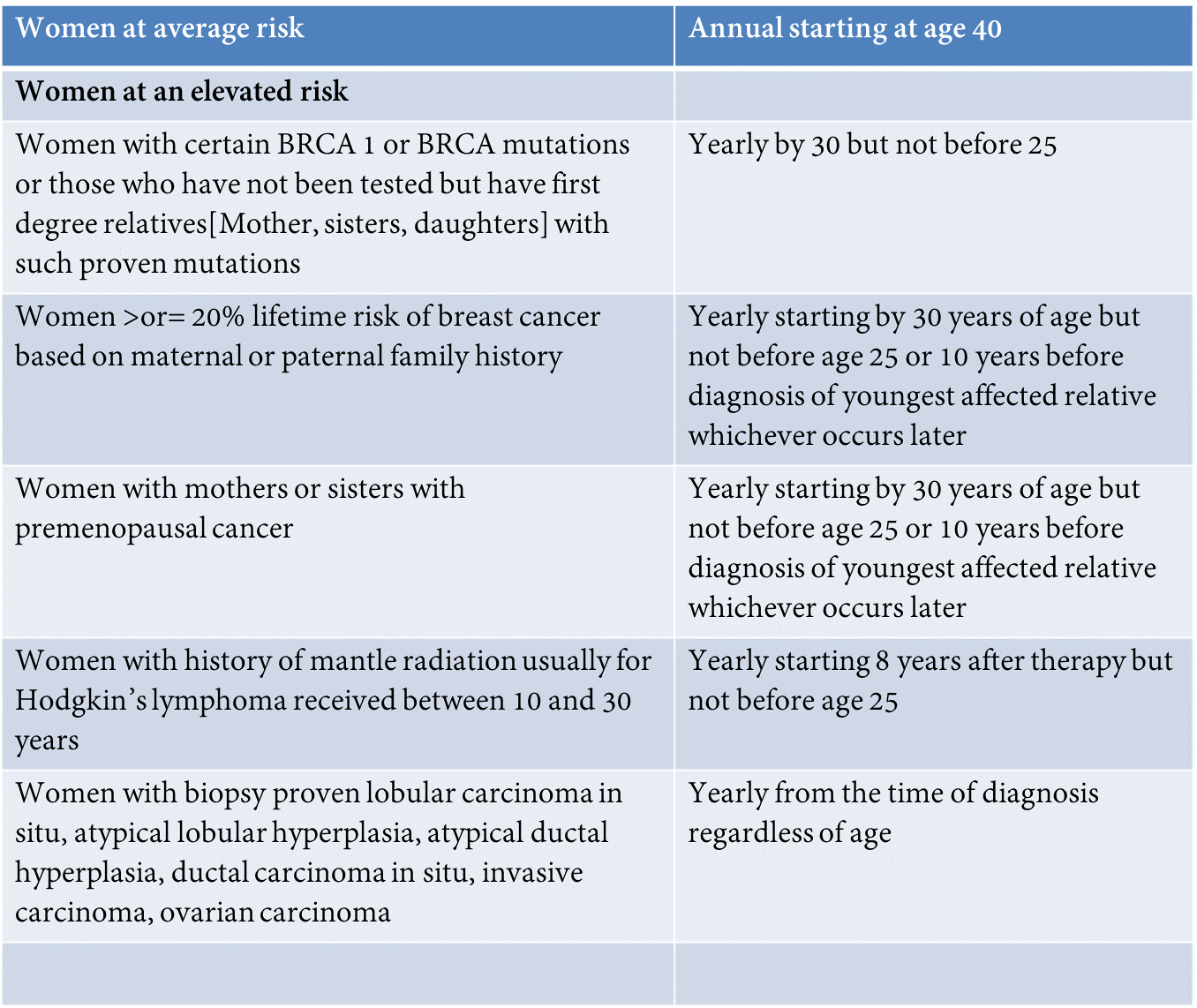
What age should women with no risk factors get mammograms ?
The American College of Radiology and the National Comprehensive Cancer Network recommend annual screening mammogram for average risk women starting at age 40 years. Those at a higher risk are advised to start at an earlier age and may need supplemental screening with MRI and or Ultrasound. See table below.
Are there alternate, better options to be screened for breast cancer?
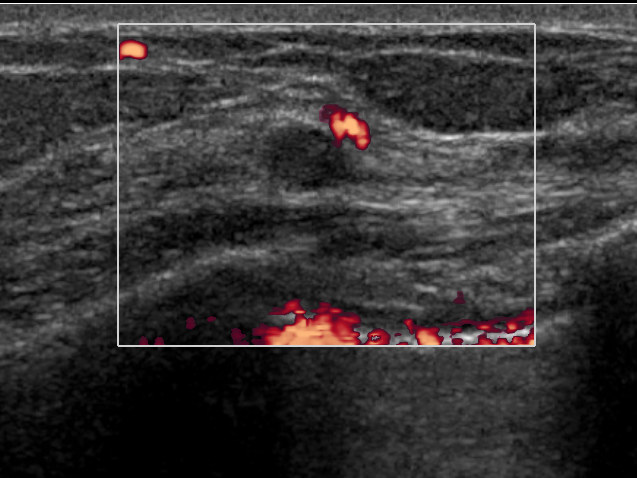
Annual ultrasound screening detects small, node-negative breast cancers that are not seen on mammography. Magnetic resonance imaging (MRI) may reveal additional breast cancers missed by both mammography and ultrasound screening. These supplemental modalities are useful in women with dense breasts and or in those who are at an increased risk for breast cancer. Figure 2.
How is the breast cancer risk assessed?
Ask your doctor about determining your breast cancer risk. There are several models in use to determine your life time risk for breast cancer. For those with a family history of breast cancer consider a consultation with a Breast Medical Oncologist to determine treatment options. Seek the opinion of a breast imaging specialist for current recommendations for enhanced screening for women at an increased risk for breast cancer. Always remember, you must be a self-advocate when it comes to your health. Breast cancer is a common disease and being vigilant and proactive is the key. The Society of breast Imaging recommends that all women undergo a breast cancer risk assessment at the age of 30 to decide a personalized an optimal screening protocol.
A useful online tool to assess breast cancer risk. https://bcrisktool.cancer.gov/
Which one to choose…3D vs 2D Mammogram
Three large prospective clinical trials have shown 3D mammogram to be 27-53% more accurate than a 2D Mammogram while simultaneously reducing false positive rates by up to 43%. 3D mammography is now the accepted standard and is currently being offered in most dedicated breast centers all over the country. State of Texas has passed a law mandating Insurance companies to cover the cost of 3D screening mammography at no cost to the insured, and also remember that screening mammogram does not require a Physician order.
Breast density and other factors that affect risk of developing breast cancer
The dense breast law requires that patients are notified of the density of their breast on a mammogram. Increased breast density means less accurate mammograms and an increased risk of breast cancer.
Increased risk of Breast cancer based on your breast density and family history:
-A woman with an extremely dense breast has twice the risk of developing breast cancer compared to a woman with scattered breast density and three times greater risk than a woman with a predominantly fat replaced breast tissue.
-Family history of breast cancer: Mother post-menopausal x 1.5 to 2
-Family history of breast cancer: Mother pre-menopausal x 3
-Family history of breast cancer: Two first degree relatives: x 3-4
-About 5-10% of breast cancers can be linked to gene mutations (abnormal changes) inherited from one’s mother or father. BRCA1 mutation have a 55-65% lifetime risk of developing breast cancer and those with a BRCA2 mutation, the risk is 45%.
What to expect after undergoing a screening mammogram:
At Pink Door Imaging, delivering accurate and prompt results is a priority so women have minimal cause to worry about the mammogram results. We have a report turnaround time of less than one business day. The recall rate is one of the lowest.
For every 100 women undergoing screening mammogram:
-About 10 women will be called back for additional imaging (False positive)
-About 2 to 3 will be recommended to undergo a biopsy
-1 out of 3-4 biopsies will be a cancer (about 1 cancer for every 200 women screened)
For every 100 women who undergo a diagnostic mammogram for a breast lump:
15 women will be requiring a biopsy and among these women 5 will have a cancer diagnosis
Every 100 women who undergo a diagnostic mammogram for a reason other than a breast lump:
9 women will require a biopsy and 3 will have a cancer diagnosis.
Debunking the Myths of the supposed harms of screening mammography:
Some of the myths associated with screening mammography is that it is harmful because of high false positive rate, high false negative rate (means that a normal mammogram does not mean that you have no breast cancer) and that it overdiagnoses breast cancer. There is also some that believe that mammography is not useful in women in their forties.
False positive results
False positives occur in about 7-10% of women screened with mammography, 80% of which are resolved with additional imaging, and 10%, with breast biopsy. How do you minimize the false positives? Choose wisely, know the credentials and expertise of the Breast Imaging specialist who is reading your mammogram.
False negative results
-An important limitation of screening is the false negatives (15%–20%). The technologic advances of digital breast tomosynthesis, breast ultrasonography, and magnetic resonance imaging counter the false negatives of screening mammography, particularly in women with dense breast tissue.• The overall sensitivity of mammography is 80%. 20% of breast cancers are not detected by mammography, but are detected by clinical symptoms such as a palpable mass or suspicious nipple discharge.
-False negatives are more likely with certain breast cancer—in particular, lobular carcinomas that tend to grow along the normal breast architecture in a lepidic pattern, making them more difficult to detect.
-False negatives are also more likely in patients with dense breast tissue, which masks breast cancer. Breast tissue density is most commonly reported using the American College of Radiology’s 4-category Breast Imaging—Reporting and Data System.
-Sensitivity is highest in the lowest density category and lowest in the highest density category, with one study showing sensitivity decreased from 87% in fatty breasts to 63% in women with the densest breasts.
Screening mammography overdiagnosis breast cancer by identifying those that do not advance and lead to unnecessary intervention and treatment.
-Medical science cannot yet determine which cancers will or will not advance to kill the person afflicted, so are you willing to take a chance and let a small early stage cancer remain in your breast because there is a small yet unknown chance that it will not grow or cause harm?
-With appropriate corrections, overdiagnosis is estimated to affect 10% or fewer breast cancers diagnosed by screening mammography
There is no benefit in screening women in their forties
-18% of breast cancers occur in women 40–49 years of age.
-One in six breast cancers occur in women aged 40-49.
-Forty percent of all the years of life saved by mammography are among women in their 40s.
-If women in the age group of 40-49 are not screened, and those 50-74 are screened biennially, approximately 6,500 additional women each year in the U.S. would die from breast cancer (AJR 2011; 196: W112–W116).
Figure 1: A 3 mm cancer found on a mammogram in a 69-year-old woman.
Figure 2: Small cancer identified in a woman with a normal mammogram on ultrasound.